Each year, approximately one in 25 American adults experience a swallowing problem[1]. This condition is referred to as dysphagia and is characterized by swallowing difficulty and/or pain or discomfort when swallowing.
Studies indicate that the prevalence of dysphagia is highest among older individuals[2]. It is estimated that dysphagia may occur in 22% of adults over 50 years of age[3] and up to 68% of residents in long-term care settings[4].
Persons with dysphagia report having difficulty swallowing food or drinks, chewing, sucking, controlling saliva, taking medication, or protecting their airway from choking. Dysphagia can occur at any time during the lifespan and may be an acute or chronic condition.
The most common causes of dysphagia are related to underlying medical or physical conditions. Individuals may have impaired swallowing secondary to a variety of challenges including reduced mastication (chewing), lost or missing teeth/dentures, and reduced oral and/or pharyngeal sensitivity typically due to an acquired event or condition like stroke, Parkinson’s disease, multiple sclerosis, or other disorders. Typically, a full assessment including a bedside swallowing evaluation, or a barium swallow study (MBS) precedes diagnosis.
Left untreated, individuals have an increased risk for developing dysphagia-related complications such as choking and pulmonary aspiration. As well, malnutrition and dehydration are of concern since the individual often will restrict food and/or beverage intake to lessen choking risk and swallowing discomfort.
Managing Dysphagia
One of the most effective ways of managing dysphagia is modifying the texture of foods (chopped, minced, pureed) and thickening liquids for the individual. This helps reduce the risk of choking or having material enter the airway.
In the past, health care providers often prescribed “mechanical soft” diets for those requiring altered consistency foods. Using this terminology to prepare appropriately textured foods and beverages continues to be challenging for providers and caregivers due to the fact there is not a universal definition for a “mechanical soft” diet.
Due to the enormous variation in types of foods and drinks, it can be challenging to categorize foods and drinks to ensure a universal understanding of the types of foods and drinks that best meet the needs of an individual diagnosed with dysphagia.
In 2013, the International Dysphagia Diet Standardization (IDDSI) committee assembled with a goal of developing international standardized terminology and descriptors for dysphagia diets that would meet the needs of individuals with dysphagia across the age span, across all care settings, and across all cultures.
In 2015, the IDDSI guidelines were published, and the “mechanical soft” diet became a relic of the past.
Dysphagia Diet
The IDDSI framework provides common terminology for describing food textures and drink thickness to improve safety for individuals with swallowing difficulties[5]
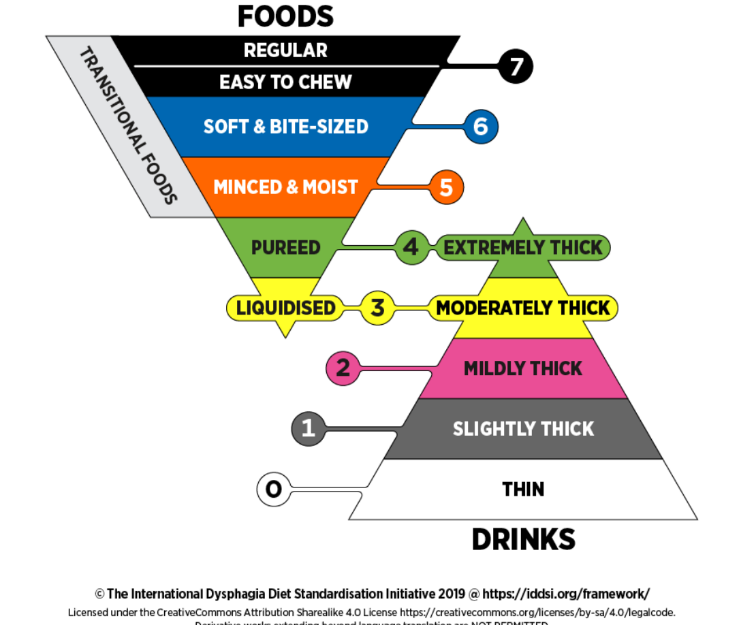
The IDDSI framework consists of a continuum of 8 levels (0 - 7). Drinks are categorized by their thickness and are assigned to a level between 0 and 4. Foods range from liquidised (level 3) to regular and easy to chew (level 7). This provides consistent terminology for providers to utilize to describe the precise level of texture modification needed for foods and thickness for drinks.
At Mom’s Meals, we have not officially adopted the IDDSI guidelines, however our pureed menu is intended to meet the guidelines of level 4 – pureed.
Mom’s Meals, at this time, does not offer specific menus for the other IDDSI levels. Most of the meals on the Mom’s Meals menus would be considered level 6 or 7, soft & bite-sized or easy to chew. To meet level 5 – minced and moist criteria, the meals would need to be mashed or chopped up further and could be easily modified to this texture with some additional manipulation.
Thickened liquids are not offered on the Mom’s Meals menus.
On occasion, clients are instructed to consume a “mechanical soft” diet to manage digestive issues associated with conditions such as ulcerative colitis or diverticulitis. Selecting meals that include soft and/or bland foods can be helpful. Clients are encouraged to experiment with meal options as individual tolerances will vary.
Mom’s Meals has a team of registered dietitians able to assist clients, caregivers, and providers in selecting the appropriate menu and meals based on individual needs. Identifying foods and beverages with appropriate texture and thickness is key to managing dysphagia. The Mom’s Meals registered dietitians are here to help clients, caregivers, and case managers select meals that are safe, balanced, and delicious. Learn more about Mom’s Meals and how our program can help support those living with dysphagia.
[1]Bhattacharyya, N. (2014). The prevalence of dysphagia among adults in the United States. Otolaryngology–Head and Neck Surgery, 151, 765–769
[2]Sura, L., Madhavan, A., Carnaby, G., & Crary, M. A. (2012). Dysphagia in the elderly: Management and nutritional considerations. Clinical Intervention and Aging, 7, 287–298.
[3] Lindgren, S., & Janzon, L. (1991). Prevalence of swallowing complaints and clinical findings among 50–79-year-old men and women in an urban population. Dysphagia, 6, 187–192.
[4]http://swallowingdisorderfoundation.com/about/swallowing-disorder-basics/
[5]https://iddsi.org/