With Mother’s Day and National Women’s Health Week right around the corner, we are focusing on the intersection of maternal health, pregnancy, and nutrition. Although pregnancy isn’t considered to be a chronic condition like diabetes, hypertension, or kidney failure, the process of carrying and birthing a child places incredible stress on a woman’s body and requires ongoing, intensive medical attention. Likewise, carrying a child for any length of time has the potential to worsen health conditions like high blood sugar, pressure, or cholesterol, or even cause them to appear for the first time.
This begs the question: are new moms getting the nutrition they need to maintain a healthy pregnancy and stable recovery postpartum? While we likely can’t answer that with a simple ‘yes’ or ‘no’, what we can do is take a look at what nutrition-related challenges – and opportunities – new mothers face in 2021.
1. COVID-19 is disproportionately affecting moms
One of the biggest lessons we learned from COVID-19 is that the virus excels at compounding existing health challenges. Working mothers especially were hit with a kind of ‘perfect storm' of challenges: a massive disruption to economic stability, childcare services, and school schedules.
Prior to the pandemic, women, more so than their male counterparts, were much more concentrated in lower-paying, face-to-face jobs (like retail and hospitality). So when the first wave of COVID arrived, women were much more likely to experience job loss and saw a 12 percentage point rise in unemployment (while men’s unemployment only rose 10 percentage points).
However, not all job loss was related to an employer’s decision to close during the pandemic – between May and June of 2020, roughly one in four women reported job loss due to a lack of childcare (twice the rate of men included in the survey).
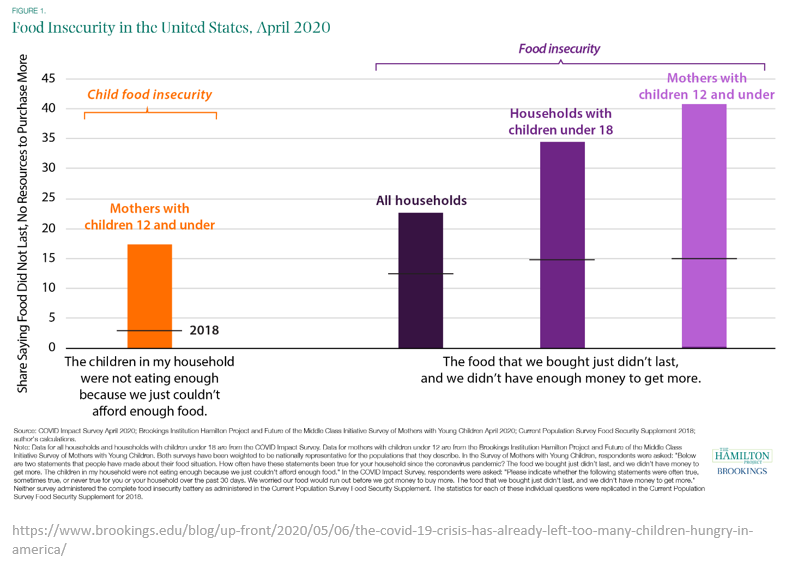
When we take these factors into consideration, we can begin to understand why rates of food insecurity, including child food insecurity, jumped dramatically during the pandemic, with mothers especially hard hit.
2. Maternal outcomes worsened during the pandemic
A woman’s body before and after delivery goes through intense physiological changes that impact their digestive, immune, and cardiovascular systems, among others. On top of that, the CDC says pregnant women are at an increased risk for more severe illness from COVID-19 when compared to non-pregnant women.
Indeed, we are already seeing a rise in maternal mortality, pregnancy complications, and stillborn deliveries during the pandemic, according to an analysis published in the journal Lancet Global Health. Part of this rise may be due to lower engagement rates between mothers and their healthcare providers, likely driven by fears of contracting the virus. Additional analysis by the CDC estimates a pregnant woman with COVID-19 has a 70% higher chance of death compared to non-pregnant women.
Prior to the pandemic, the United States’ maternal mortality rate was already on the rise: 20.1 deaths per 100,000 live births in 2019 marked a 15% increase from the previous year. If this sounds high, it’s because it is – relative to other developed countries, the U.S. ranks highest in number of maternal deaths during childbirth, with 2/3 of them considered preventable.
When you throw food insecurity into the mix, you increase the mother’s chances of experiencing gestational diabetes, hypertension, pre-eclampsia, and other health factors that put the lives of mother and baby at risk. Likewise, poor nutrition increases the risk of infant mortality, low birth weight, birth defects, and other adverse outcomes for the baby.
When you consider that cardiovascular disease and endocrine disorders, which are both closely linked to diabetes and obesity, are the top two leading causes of maternal death in the U.S., we can begin to see how nutrition insecurity and the pandemic’s socioeconomic impacts are putting American mothers in a vulnerable situation.
3. COVID-19 is widening maternal health disparities (but help may be on the way)
The CDC analyzed characteristics of SARS-CoV-2-positive pregnant and non-pregnant women of reproductive age and noted several instances where women of color faired worse, according to a summary report.
For example, although only 14.1% of the women included in the analysis identified as Black, they made up 26.5% of deaths among pregnant women and 37.4% of deaths among nonpregnant women. The CDC also found that, among Hispanic women, pregnancy was associated with 2.4 times the risk for death.
“Regardless of pregnancy status, non-Hispanic Black women experienced a disproportionate number of deaths relative to their distribution among reported cases,” the article states. “This analysis highlights racial and ethnic disparities in both risk for infection and disease severity among pregnant women, indicating a need to address potential drivers of risk in these populations.”
Those potential drivers of risk include chronic conditions such as diabetes and heart disease, which both occur at much higher rates among Black and Hispanic women, due in part to both biological risk factors and social determinants of health (SDOH).
Lawmakers have recognized this complex health disparity and are reviewing a proposed piece of legislation known as the Black Maternal Health Momnibus Act of 2021, which combines 12 separate proposals all designed to address different aspects of the maternal health crisis in America, including several proposals to expand existing nutrition programs and create new ones.
The Road Ahead
The COVID-19 pandemic has challenged us all to find new ways to care for others and address long-standing issues such as health inequity and hunger. While the rise in vaccines and virtual care is encouraging, these tools alone won’t be enough to solve one of our most basic human needs: access to nutritious, healthy food.
We’ve worked with several health plans across the U.S. to design and implement a home-delivered meals program tailored to high-risk pregnancies, including those with a current case (or high risk) of gestational diabetes.
Join us for our upcoming webinar “Enhancing Maternal Health with Home-Delivered Meals”, delivered in partnership with Florida-based Simply Healthcare, made available through Medicaid Health Plans of America.
Learn more about nutrition’s role in pregnancy, or how you can connect people in your community with home-delivered meals. Contact us today.