Want to cut hospital readmissions? Focus on the fridge.
Unplanned hospital readmissions in the U.S. cost between $15 and $20 billion annually[i]. Common causes for readmission include premature discharge, infections, complexities from having multiple chronic conditions, and taking high-risk medications. But there are several harder to identify social risk factors including financial security, access to food, housing and employment, commonly known as Social Determinants of Health (SDOH), that drive up hospital readmissions.
The SDOH connection
Tackling the impact of SDOH on all facets of health care including readmission rates is a hot topic for health plans, health systems, and government agencies. But these social risk factors have been long-standing problems underlying our health care system. Under-addressed until relatively recently, SDOH have cost patients time in recovery and they’ve taken an enormous financial toll on the health care industry and tax payers.
A recent study by Waystar, which produces revenue cycle management solutions, shows that 68% of consumers are dealing with some level of SDOH, and 52% report being high risk in at least one facet of SDOH.[ii]
Studies show a clear link between SDOH and worse clinical outcomes, particularly hospital readmission rates.[iii] The reasons for this tight correlation are complex and aren’t fully understood, but include transportation problems that lead to missed follow up appointments, inability to afford medicines prescribed to help the patient heal at home, and poor adherence to self-care regimens which hampers the healing process.
A study found that hospitals that treat the most vulnerable patients could reduce penalties under Medicare’s Hospital Readmission Reduction Program (HRRP) by 21.8% if CMS adjusted hospital readmission rates to include SDOH on the patient level.[iv]
Fortunately, if a patient’s SDOH risk is identified, it can often be addressed. Health plans and hospitals around the country are developing unique – and effective -- approaches to recognizing high risk patients and mitigating their social risk factors so they can heal, remain healthy -- and stay out of the hospital.
Food as medicine
One Maryland hospital cut its readmission rate in half for high-risk patients while also reducing spending by 35% on hospital costs for that same group.[v] The University of Maryland St. Joseph’s Medical Center partnered with Maxim Healthcare Services to provide community health workers who address SDOH for high-risk patients in their homes. They looked at non-clinical barriers that stop patients from following their care plans including transportation and housing issues, employment, even access to healthy food. Then they leveraged community resources to help address the identified problems. The program reduced readmissions and saved the hospital more than $3 million over two years.
Other health plans are taking more targeted approaches, for instance, having clinicians write prescriptions for healthy food or adding meal benefits to health benefits packages. When it comes to hospital readmission rates, improving nutrition alone can have a big impact. One study in Philadelphia, showed that medical costs for patients who received nutritious, home delivered meals were cut by $12,00 a month per patient mainly due to lower hospital admission costs[vi].
Additional research supports nutrition’s key role in the likelihood of hospital admission, length of stay, and readmission. According to one study in the Journal of Primary Care and Community Health, better nutrition reduced hospital admissions by 7 percent for people with diabetes and by 50 percent for people with multiple conditions. Once the patient is discharged from the hospital, access to good nutrition can cut readmission rates.
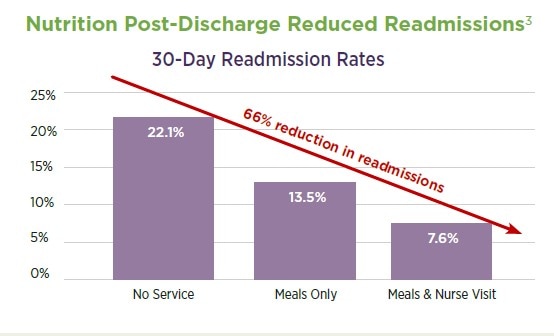
Through our post-discharge program, Mom’s Meals delivers refrigerated, condition-appropriate meals to patients around the nation, providing expedited nutritional support at the start of their recovery, when time is of the essence, to support healing and reduce readmissions. Click here for more information.
_________________________________________________________
[i] https://www.uptodate.com/contents/hospital-discharge-and-readmission
[ii] https://www.healthleadersmedia.com/finance/5-ways-social-determinants-health-affect-revenue-cycle
[iii] https://onlinelibrary.wiley.com/doi/full/10.1111/1475-6773.13133
[iv] https://revcycleintelligence.com/news/social-determinants-of-health-impact-hospital-readmission-rates
[v] https://homehealthcarenews.com/2019/02/home-health-partnership-cuts-re-hospitalizations-in-half-reduces-spending-by-35/
[vi] https://www.forbes.com/sites/sachinjain/2019/04/07/sometimes-food-is-the-best-medicine/#2fc3cfd7186b